Preventing Stroke From Every Level using an Integrated Socio-Environmental Model of Health
- jaimielmarchand
- Nov 8, 2021
- 5 min read
Emergency Departments (ED) take pride with being skilled at rapid recognition, diagnosis, and treatment of disease presentations to maximize health outcomes for patients. Stroke and Heart Disease are two of the most common conditions encountered in the ED. Baptiste et al state, "Persons with coronary heart disease (CHD) or stroke demonstrate a high frequency of emergency department visits to manage acute and chronic symptoms", and, "Frequent emergency department visits may reflect disease progression and poorly controlled chronic conditions" (2021). These statements reflect how these two chronic diseases can present as acute, or progressively worse depending on individual and health determinants involved.
Alberta Health Services (AHS) state that, "approximately 30 per cent of Albertans report having at least one chronic health condition and that number increases to over 75 per cent if you are 65 years of age and older" (2021). The Report on the Auditor General of Alberta reports, "In Alberta people with chronic disease account for nearly two-thirds of hospital inpatient stays, one-third of all visits to physicians, and more than one-quarter of visits to emergency" (2014) which highlights the need for prevention plans and strategies to decrease risk and onset of disease.
The World Health Organization (WHO) reports, "the most important behavioral risk factors of heart disease and stroke are unhealthy diet, physical inactivity, tobacco use, and harmful use of alcohol" (2021). MyHealthAlberta mirrors the WHO and recommends, "Lifestyle changes including quitting smoking, eating heart-healthy foods, getting regular exercise, staying a healthy weight, lowering stress level, and limiting alcohol intake" (2021) as ways to decrease risk of heart disease and stoke.
Emergency Departments often treat the worst-case scenario of chronic disease, for example acute stroke and acute myocardial infarction. Treatment is provided based on evidence-based, best practice guidelines provided by AHS, "Alberta's stroke prevention and treatment programs are recognized as among the best in Canada", and, "AHS' acute care protocol has enabled stroke teams to provide treatment more promptly for patients across the province, giving them their best chance for a full recovery"(AHS, 2021).
Disease prevention measures such as eating heart healthy foods, daily physical activity, and avoidance of tobacco and alcohol should be adopted at a very young age. Healthy habits will lead to a healthy lifestyle and decreased risk of developing a chronic disease. Opportunities to be healthy are closely linked to the conditions in which people grow up, learn, live, work and age (WHO, 2021). Unfortunately, not everyone has the experience of growing up in a home and community that supports and promotes healthy habits and lifestyle. Education, food, housing, and early childhood development are some of the social determinants of health listed by the WHO, “social determinants of health account for 30-55 per cent of health outcomes” (2021), and while healthy habits begin at the individual level, there is need for multilevel involvement and intervention in order for equitable access to information and resources for all Canadians.
Alvarez et al propose an integrated socio-environmental model of health and well-being intended to reach socially disadvantaged individuals and populations, “Researchers evaluating social and environmental determinants of disease have historically worked in parallel with little crossover despite a common goal of promoting and safeguarding human health. Social and environmental risks do not exist in isolation but rather co-occur and affect socially disadvantaged individuals and populations experiencing health disparities” (2018). Their approach focuses on factors within the environment that impact health, factors that increase disease risk and also factors that are protective to a healthy state. The model they developed is termed the Integrated Socio-Environmental Model of Health and Well-being (ISEM), “it is designed to have broad applicability across populations and life stages” (2018).
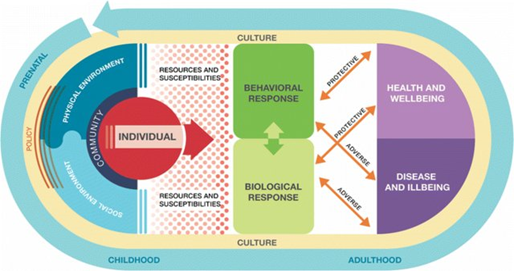
The ISEM “begins at the individual level (i.e. sex, age) as well as community level, which is further embedded in a larger social and physical environment shaped by both policy and culture” (Alvarez et al, 2018).They explain that, “communities are comprised of culturally based norms and practices that can be shaped by the larger social and environmental contexts”, and, “Thus intra-individual, community-level, social, and physical environmental factors independently and jointly play a role in the health of individuals” (2018). Furthermore, the ISEM highlights how individuals are embedded within communities and may adopt the culture of the community, which can lead to negative or positive outcomes depending on community’s culture, “culture refers to collectively held behavioral norms, traditions, worldviews, and beliefs, which may shape socio-environmental factors and their health effects in systematic ways” (Alvarez et al, 2018).And finally on a larger scale the ISEM, “recognizes that policy shapes various aspects of both the social and physical environment” (Alvarez et al, 2018).This model identifies the many levels involved with addressing social determinants of health, and how each level may respond to decreasing risk of disease and chronic disease within a population.
Applying this model to a chronic condition such as stroke with a focus on preventative measures and lifestyle changes can effectively decrease risk of disease and disease progression, decrease visits to physicians, emergency departments & hospitals therefore decreasing costs related to healthcare, and increase quality of life at all stages. Beginning at the individual level, one can make decisions that support a healthy behaviors and positive outcomes.
Heart & Stroke suggest that, “prevention is key and starts with knowing your risk”, and, “80 per cent of premature stroke and heart disease can be prevented through healthy behaviors such as eating healthy, being active, and living smoke free” (2021). An adult has the capacity to make these decisions, but to promote these behaviors at a young age, they need to be taught and role-modelled, and have community resources available to support these healthy behaviors. For example, a family of two adults who exercise regularly, choose healthy foods with plenty of fruits and vegetables, do not smoke, and live in a community that provides access to walking/bike trails, recreational centers and sports fields, farmer’s markets with fresh produce and grocery stores, and also project these behaviors to their children will, in theory, have decreased risk of developing conditions that lead to a chronic disease such as stroke.
In comparison, the same family of two adults with children living in a community that does not support healthy behaviors, eats high fat foods, smokes tobacco, and does not exercise will be at higher risk of developing stroke or other chronic diseases. Alvaraz et al report, “research has consistently demonstrated that a poor neighborhood food environment defined according to level of availability and accessibility to healthy food are significant risk factors for obesity” (2018) a condition that is defined by Kernan et al as, “a highly prevalent risk factor in stroke” (2012).
The ISEM can be used to guide community populations toward an overall healthier state, and uses the example, “neighborhood zoning policy could directly affect the density of alcohol outlets, availability of grocery stores, and access to safe and affordable in communities” (Alvarez et al, 2018). A neighborhood zoning policy that supports healthy lifestyles can provide a trickledown effect of healthy communities and decreased risks for disease to these populations which lead can to decreased strain on the healthcare system, and overall decreased need for spending in the healthcare system.
In summary, the ISEM supports application of health promotion strategies at all levels including individual, community, and government with social and environmental consideration. Many of the social determinants of health as listed by the WHO that have been identified as risk factors for the development of chronic disease have been incorporated into the ISEM with suggestions and recommendations of how to mitigate development of healthy habits that will decrease the risk of chronic disease such as stroke beginning at a young age and throughout the life span.




Comments